Some portions of our bodies tend to get more attention than others when we talk about them. Consider the arms, legs, face, and even the abdomen. The gluteal cleft is one area that is frequently disregarded and infrequently mentioned. The gluteal cleft, also referred to as the “butt crack,” is a crucial anatomical feature, and being aware of it can help you take better care of yourself and maintain better overall health.
Overview about Gluteal Cleft
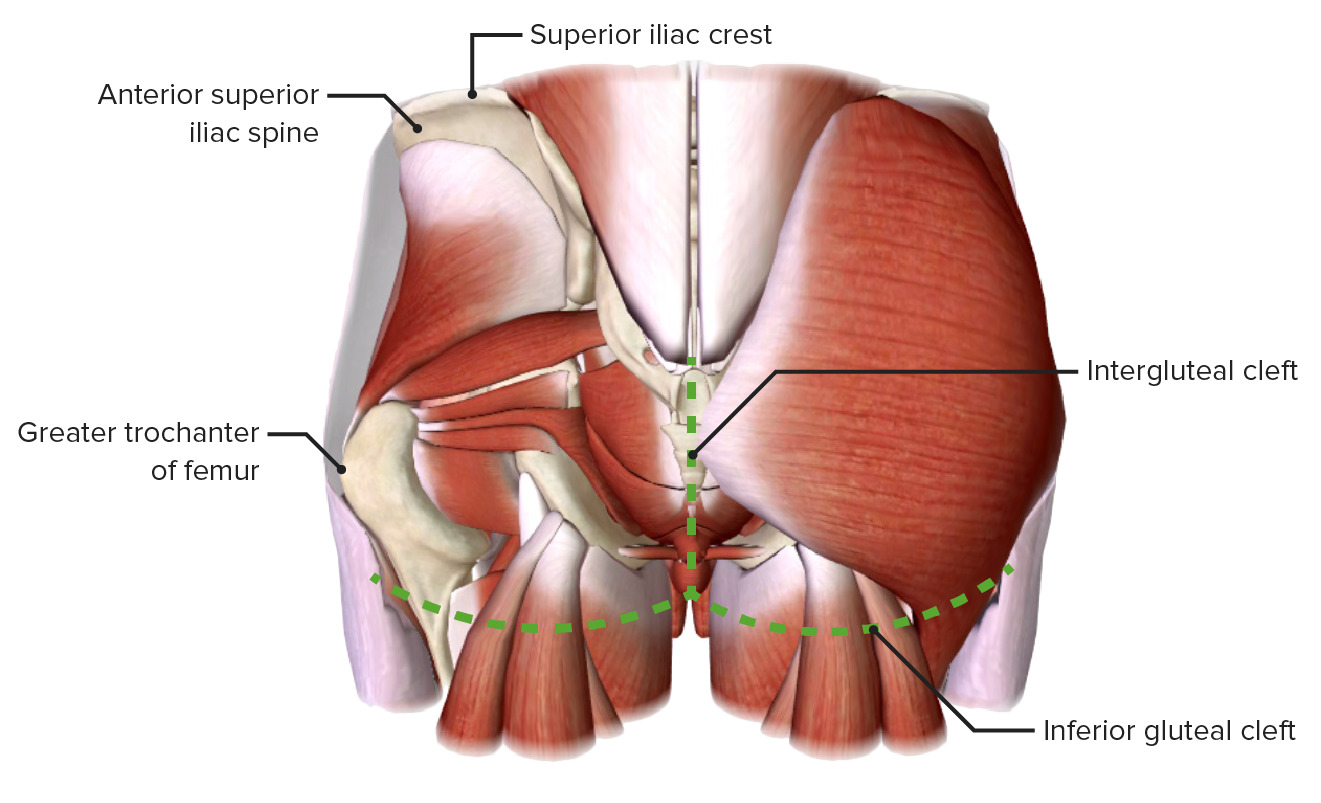
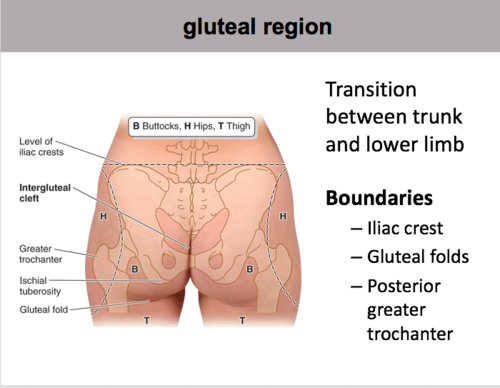
The groove between the buttocks, running from the base of the spine to the anus, is known as the gluteal cleft. The gluteus maximus, which makes up the majority of the buttocks, is one of the two gluteal muscles that it divides. Despite having a seemingly modest structural role, the gluteal cleft has a number of crucial functions.
One of the key justifications for paying attention to the gluteal cleft is hygiene. Because of its natural warmth and frequent moisture from perspiration, this area is a haven for bacteria and fungi. Poor or insufficient gluteal cleft cleansing might leave behind offensive odors, rashes, or even infections. Regularly cleaning with mild soap and water and thoroughly drying afterward might aid in maintaining excellent hygiene and avert pain or health problems.
The hair follicles are another feature that is intimately connected to the gluteal cleft. As a barrier of defense, the hair in this region lessens friction and prevents chafing. But abundant hair can also collect bacteria and perspiration, increasing the likelihood of skin discomfort. If there is a lot of hair around the gluteal cleft, people may choose to clip it or use hair removal techniques that don’t raise any hygienic issues.
The gluteal cleft is essential for responding to pressure and weight distribution in addition to maintaining hygiene. The gluteal cleft relieves pressure on the tissues between the buttocks while one is sitting or lying down, which lessens pain and promotes better blood flow. Without the gluteal cleft, people would be more uncomfortable in certain positions, which could result in pressure sores or bedsores.
In addition, the gluteal cleft is a crucial region for body aesthetics. The attractiveness of a well-shaped posterior has drawn a lot of attention in contemporary countries. The gluteal cleft’s contour and depth influence how the buttocks seem as a whole. Understanding the gluteal cleft can assist people in concentrating on exercises and other activities that strengthen their gluteal muscles, which will eventually result in a more toned and appealing appearance.
In addition to its practical uses, the gluteal cleft has long had symbolic and cultural significance. It is portrayed in literature and art in certain civilizations as a highly eroticized locale. The gluteal cleft is a feature of beauty that has long been appreciated by artists, including painters and sculptors, who have used it as a focus point in their creations. Understanding this historical background might help one appreciate the beauty and uniqueness of this much undervalued body component more deeply.
The gluteal cleft is much more than simply a basic groove between the buttocks, to sum up. Basic hygiene, weight distribution, and even cultural significance are just a few of its many roles. The gluteal cleft can be properly managed and understood to prevent pain, improve physical appearance, and advance general wellbeing. The next time you catch a glimpse of your gluteal cleft, keep in mind that it is important and that you should treat it as such because even the seemingly unimportant portions of our bodies have meaning and deserving of our attention.
Gluteal cleft causes
- Genetics – Some people are simply born with a deeper or wider gluteal cleft due to their genes, and this is completely normal.
- Overweight – People who are overweight or obese may have a deeper gluteal cleft due to excess fat deposits in the area.
- Poor posture – Poor posture can cause the muscles in the gluteal region to weaken, which can create a deeper cleft.
- Aging – As people age, the skin and muscles in the gluteal region can become less elastic, which may cause a deeper cleft.
- Hormonal imbalances – Hormonal imbalances can cause changes in the skin and muscle tissue in the gluteal region, which may lead to a deeper cleft.
- Infection – In rare cases, infections in the gluteal region may cause scarring or damage to the skin and muscle tissue, leading to changes in the appearance of the gluteal cleft.
Why is my intergluteal cleft painful?
The intergluteal cleft, sometimes known as the “butt crack,” can hurt for a number of different causes. Here are some potential reasons:
- Pilonidal cyst: This cyst often develops in the intergluteal gap, close to the tailbone. It frequently comes from an infection or an ingrown hair, and it hurts and is uncomfortable.
- Chafing or friction: Constant rubbing of the skin in the intergluteal cleft, particularly when jogging or walking, can cause irritation, friction, and ensuing pain.
- Dermatitis: The intergluteal cleft may be affected by skin disorders including contact dermatitis or psoriasis, which can lead to redness, itching, inflammation, and discomfort.
- Infection: In the intergluteal gap, bacterial or fungal infections can manifest as pain, itching, and inflammation. Examples include fungal infections like jock itch or bacterial folliculitis.
- Hemorrhoids: In certain instances, uncomfortable and painful hemorrhoids can expand from the anal region into the intergluteal gap.
It is advised to see a medical professional for a precise diagnosis and the best course of therapy if you are dealing with chronic or severe pain.
Identifying Skin Breakdown in the ‘Gluteal Cleft’
The CDC reports that the prevalence of obesity in the US has increased to 42.4% and that medical expenses have surpassed $1 billion. Taking care of this patient population has special difficulties, notably with regard to skin deterioration. Pressure wounds do not usually develop in the typical places, such as the heels and sacrum. That is too simple. They can occasionally be found in difficult-to-reach places like the gluteal cleft. However, just because these wounds are hard to access does not mean that they should be disregarded.
Patients with solid buttock tissue who are obese are especially vulnerable. Skin breakdown may occur if doctors are unable to separate the gluteal cleft in order to examine the skin’s integrity or clean and dry the area. But first, it’s critical to comprehend the distinction between skin harmed by moisture and pressure injuries.
As MASD (moisture associated skin damage), moisture-related skin breakdown is typically characterized by superficial skin loss and uneven margins. Acute maceration can happen when the skin is exposed to a lot of wetness for an extended period of time. The outer layer of epidermal cells overhydrate, which results in swelling and reduces the skin tissue’s resistance to injury. When the epidermis’ outer layer is removed, the pain and danger of secondary bacterial and/or fungal infections increase.
It is appropriate to classify linear lesions in the intergluteal cleft as intertriginous (between skin folds) dermatitis since they are brought on by moisture with or without a friction component. But pressure wounds, which affect the skin and underlying soft tissue, are ischemic wounds that may cause full-thickness tissue destruction. Pressure and shear factors impede blood flow, distort blood vessels and tissue, and harm tissues during reperfusion, all of which contribute to the emergence of pressure injuries. So, how should the gluteal cleft problem be solved?
The first step in prophylaxis is to be aware of the potential for pressure injury to develop in patients with a firm inter-gluteal cleft. It is crucial to be aware. Regularly inspecting the gluteal cleft with care is crucial, as is palpating the area to check for soreness and bogginess. Additionally, in this patient population, it could be necessary for two caregivers to help with the skin examination. The best course of action is to start implementing pressure redistribution support surfaces for those who are at risk and solid treatments to regulate moisture. Don’t forget the chairs, though. People with compromised health need to be protected both in and out of bed. Match the product to the patient to find the best support options for any patient population!
What causes skin to split between buttocks?
Common skin conditions that can result in split or damaged skin between the buttocks include:
- Dry skin: Dryness and cracking of the skin can be caused by a lack of moisture. This might be caused by psoriasis, eczema, or over-bathing or sweating.
- Friction: Regular skin-to-skin contact in the intergluteal cleft, particularly during strenuous sports like jogging or cycling, can result in abrasions that tear the skin.
- Fungus infection: In the warm, moist environment of the intergluteal gap, a fungus such as jock itch can form, causing cracking and itching.
- Yeast infection: Yeast can develop in the skin’s folds and result in intertrigo, a condition that can cause cracking, itching, and pain.
- Other skin problems: Other skin conditions that can divide the skin between the buttocks include lichen sclerosus, inverse psoriasis, and seborrheic dermatitis.
Split skin can be unpleasant and uncomfortable between the buttocks. If the condition persists or gets worse, it is advised to go to a doctor. A medical expert can conduct a physical examination and make suitable therapy recommendations.